Picky Eaters? Family Strategies for More Peaceful Meals

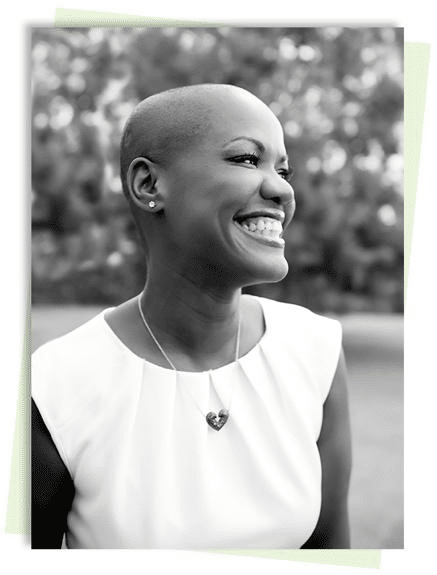
If your child is a picky eater, it can be tough on your whole family. Not only do parents worry that their child isn’t getting enough nutrients for healthy growth, but many picky eaters get anxious and even throw tantrums at mealtimes to avoid foods they don’t like. At No Limits Pediatric Therapies in Bentonville, AR, our mission is to help children reach their fullest potential through play-based therapy solutions. Today, I want to share some strategies to make mealtimes more peaceful for families dealing with picky eaters. Simply Forcing Kids to Eat What Is Offered Is Not Effective Many children who are picky eaters struggle with an underlying condition that can make it difficult for them to tolerate the textures, tastes, or smells of different foods. These conditions can make mealtimes stressful, and forcing children to eat what’s on their plate can lead to meltdowns and increased anxiety around food. Understanding the underlying issues and how to help children overcome them can make mealtimes calmer and more effective for families. What Is Avoidant/Restrictive Food Intake Disorder (ARFID)? Avoidant/Restrictive Food Intake Disorder (ARFID) is a condition where children have a lack of interest in eating, sensory sensitivities, or fear of eating due to frequent choking or vomiting on their food. It’s a condition that often accompanies autism, as children with autism can struggle a lot with sensory sensitivity. Common signs of ARFID include: A noticeable lack of appetite Avoiding foods with certain textures or colors Significant weight loss or nutritional deficiency Constipation, stomach pain, or cramps Excessive tiredness Muscle weakness Try the “One Safe Food” Strategy One effective strategy for managing ARFID is to include at least one “safe” food in every meal. A safe food is something your child reliably eats without issue. By including this option, children can feel a sense of success and reduce their anxiety about trying new foods. This is because they may not be able to eat much of the new foods you are introducing, but they will be able to fall back to their safe food if it’s available on their plate. This positive reinforcement can gradually encourage them to be more open to trying other foods on their plate. Additionally, giving them their safe food will ensure they do get some nutrients, which is important for their overall health and wellbeing. Limit Quantities of Challenging Foods To avoid overwhelming your child, limit the quantities of challenging foods on their plate. A large portion of foods they dislike or are reluctant to try can be overwhelming and may cause them to shut down. It can make them feel like the obstacle is too difficult to overcome and they’ll never be able to do it, so what’s the point in trying? Instead, keep challenging foods in very small portions and separate them from your child’s safe food. This approach helps children feel more comfortable and less pressured during mealtimes, which can make it easier for them to consider trying new foods. Reach Out to No Limits for an Evaluation If mealtimes are a constant struggle in your home, our pediatric therapists can help. Give us a call at (479) 250-9838 for a free 15-minute developmental consultation. We’ll help determine if your child might benefit from pediatric therapy and work with you to make mealtimes a more peaceful and enjoyable experience for your family. About Terrica Terrica Weatherford, MSOT, founded No Limits Pediatric Therapies in 2016. She earned her Master of Science in Occupational Therapy from the Medical University of South Carolina in 2012. For over 13 years, Terrica has been committed to helping neurodiverse children (and those who need extra support) reach their full potential. She founded her practice to ensure she could provide exceptional care for children and their families.
Concerned You Waited Too Long to Get Your Child to Therapy?

Many parents don’t realize that their child needs developmental support until they start having trouble in school. But by that point, they often worry that they are too late to get their child the help they need to thrive. At No Limits Pediatric Therapies in Bentonville, AR, our goal is to support children in reaching their fullest potential, no matter when they begin their therapy journey. Today, we want to address a common concern many parents have: “Is it too late to start therapy for my child?” Every Family’s Journey Is Unique No two families are the same, and each child’s therapy journey is unique. Pediatric therapists understand that the needs of each family and child differ when they start care. There is no “one size fits all” approach, and most importantly, there is no deadline to receive therapy. Our approach is to meet each family where they are by addressing their specific concerns. No matter how young or old your child is, pediatric therapy is tailored to fit their unique circumstances and help them achieve their developmental milestones. Treatment Begins with an Assessment of Current Developmental Progress and Delays The first step of treatment at any pediatric therapy clinic is a thorough assessment of your child’s current abilities and areas for improvement. Our job is to evaluate your child’s skills compared to the common developmental milestones for their age. This process allows us to gather essential information so we can fully understand and meet your child’s needs. The initial assessment is a crucial part of your child’s therapy journey, as it lays the foundation for creating an effective treatment plan tailored to their specific developmental challenges. A Therapeutic Program Is Customized to Each Child’s Needs Based on the initial assessment, our pediatric therapists will develop a customized therapeutic program designed to meet your child where they are developmentally. This individualized treatment plan aims to help your child gradually build up their skills so they can achieve greater developmental milestones. By focusing on your child’s unique strengths and areas for growth, we can provide targeted interventions that empower their development. With pediatric therapy, you can help your child overcome any challenges they may face in daily life. The Right Time to Start Is as Soon as Developmental Problems Surface Parents know their children best and have invaluable insights into their child’s development. If you have any concerns about your child’s development or notice any struggles they have in daily life, we do recommend that you get a pediatric therapy evaluation as soon as possible. This is because the earlier developmental delays are addressed, the easier they are to manage. However, that doesn’t mean that it’s ever “too late” for your child to receive support. Parents, like all of us, are only human, and sometimes we miss things. Or sometimes we take a “wait and see” approach in hopes that the delay will improve with time. The important thing to remember is that there is not a limited window of time where your child can benefit from pediatric therapy. The best time to seek pediatric therapy is as soon as you notice something is not quite right. The second-best time is now. Our advice to you is to trust your instincts and reach out for help, no matter how young or old your child is. Reach Out to No Limits for an Evaluation If you are concerned about your child’s development, don’t hesitate to reach out to our team at No Limits Pediatric Therapies. We offer a free 15-minute developmental consultation to help you determine if therapy is the right step for your child. Call us today at (479) 250-9838 to schedule your consultation and take the first step towards helping your child grow beyond their limitations. About Terrica Terrica Weatherford, MSOT, founded No Limits Pediatric Therapies in 2016. She earned her Master of Science in Occupational Therapy from the Medical University of South Carolina in 2012. For over 13 years, Terrica has been committed to helping neurodiverse children (and those who need extra support) reach their full potential. She founded her practice to ensure she could provide exceptional care for children and their families.
Activity Level vs. Arousal Level? What does it All Mean?
If you have been around No Limits Pediatric Therapies long, you have probably heard the terms AROUSAL level and ACTIVITY level; but what do these terms really mean? Let’s go to one of No Limit’s OT teams favorite sensory gurus named Dr. Julia Harper for some more information. Dr. Julie Harper, PhD, MS, OTR/L is a wife, mother, occupational therapist, business owner, psychologist, life coach & mentor, speaker and writer. She holds a BS in Occupational Therapy from SUNY Health Science Center (Downstate), Brooklyn, NY, a MS in Occupational Therapy from Boston University, Boston, MA and a PhD in Psychology from Capella University, Minneapolis, MN. She brings all of these roles together to serve her mission of helping people-all people to live their lives beyond limitations. For over 20 years, Julia has worked as a pediatric occupational therapist focusing on creating brain-based therapeutic programs that tap into neural-plasticity, the brain’s ability to adapt and change. Her world-renowned therapy center offers a W.A.Y. to H.O.P.E.™ which merges her two models: HOPE (Harper’s Optimal Protocols for Enrichment), which focuses on re-wiring the brain of those with physiological, learning and limitations in attention and W.A.Y.™ (What About You), which retrains the brain to move beyond emotional and thought limitations. Creating change is at the center of her work, as she knows that to best serve the world, she needs to be an agent of change. This begins with the work she has done to change her own life, from becoming a Certified Master Life Coach, a Master Clinician, a Certified Daring Way Facilitator and Master Practitioner of MER. She hopes that through her change, she can change her clients and have the ripple effect of changing the world. She is a firm believer that all change begins with her. Daily, she lives this change to be the change. (http://therapeeds.com/en/about-us/julia-s-story) Now you know a little background on one of our favorite resources when it comes to sensory processing, arousal level, and activity level, but what does it all mean? Activity level can be broken down into two categories: high activity and low activity. When speaking about activity level, we are referring to physical activity. The World Health Organization defines physical activity as any bodily movement produced by skeletal muscles that requires energy expenditure. Physical activity refers to all movement including during leisure time, for transport to get to and from places, or as part of a person’s work. Both moderate- and vigorous-intensity physical activity improve health (https://www.who.int/news-room/fact-sheets/detail/physical-activity). This is leading to the idea that a child or adult who demonstrates a high activity level demonstrates significant physical activity and seeking of movement. It then leads us to an idea of a child or adult who demonstrates a low activity level demonstrates minimal physical activity at any given time. Activity level is visible, fluid and changing. You can move from high to low activity level or low to high activity level at any point in the day and it usually changes multiple times during a day. It can even change hour to hour or in shorter time spans. Remember, activity level is seen and is changing; although you may have a child who typically demonstrates either a high or low activity level. Now, let’s move on to arousal level. This can easily be confused with activity level, but it is different and cannot be used interchangeably. Your arousal level tends to remain unchanging and can be considered more as your state of being. With that said, according to Julia Harper, a child or an adult can be considered high arousal or low arousal. She describes the different neuro-chemicals and brain wave patterns within the body that determine arousal level, but that will be left for another day. What we will discuss today is that depending on your child’s arousal level, the occupational therapy team can better serve your child’s sensory needs by meeting their specific sensory input needs. This is based on neuro-chemical needs and we can then help create a protocol to meet those needs based off of Julia Harper’s research. Moving forward, let’s discuss how we determine if your child is high arousal or low arousal. We can typically describe a high arousal child as a child who thrives on routine, structure, and predictability. A high arousal child is unable to start off their day with intense sensory input such as spinning and participating in inverted activities, because intense vestibular input is only going to dysregulate your child even more. This would be working against the whole goal of working with your child to build a toolbox to help improve attention, participation and overall regulation based on their individual arousal level. They tend to benefit from deep pressure touch and passive proprioceptive input which is calming and regulating. Now on the other hand, you have a low arousal child. A low arousal child is a child who tends to be unpredictable, constantly changing, and unrhythmical. You can usually see this in everything they do. A low arousal child may always be on the go because they are seeking input to help regulate, but they do not need to start the day off with calming activities. Instead, they need to start off with intense vestibular input that is constantly changing, unrhythmical and unpredictable. Starting with intense input followed by deep pressure and tactile input will help set your low arousal child up for success. Now, here is where it gets tricky! Is my child high or low arousal? Or are we just looking at if they have a high or low activity level? This is where your OT comes in. We at No Limits want to work with you as a family and complete a variety of clinical observations to help determine if your child is high or low arousal. We can then work with you to see how their activity level usually runs at different points in the day. After determining your child’s arousal level and gaining a better idea of how their activity
Occupational Therapy and the Adolescent Years
Adolescent years bring about many changes including taking on responsibilities in the home, more demands at school, employment, driving, bodily changes, relationships, money management, increasing independence as they prepare for adulthood, and more. Occupational therapists come alongside adolescents to help support and increase their independence in these daily occupations, or everyday activities one engages in. More specifically, within the OT Practice Framework (AOTA, 2014), daily occupations consist of ADLs and IADLs. Activities of daily living (ADLs) are considered to be nine activities: bathing/showering, toileting and toilet hygiene, dressing, swallowing/eating, feeding, functional mobility, personal device care, personal hygiene and grooming, and sexual activity; whereas, instrumental activities of daily living (IADLs) encompass 12 activities that “require more complex interactions than those used in ADLs” including care of others, care of pets, child rearing, communication management, driving and community mobility, financial management, health management and maintenance, home establishment and management, meal preparation and cleanup, religious and spiritual expression, safety and emergency maintenance, and shopping (AOTA, 2014, p. S19). An occupational therapy session with this age group can include so many functional, important skills, while keeping the session fun! When working with adolescents, a treatment session might include activities such as hygiene tasks including brushing teeth, applying deodorant, nail trimming, and combing hair, dressing skills, simple household chores such as separating and completing laundry, bed making, loading and emptying a dishwasher, sweeping, or vacuuming, meal prep and cleanup, and kitchen and food safety. Other sessions might include walking to a nearby restaurant or store to complete a point of service transaction to purchase items, going for a walk outside to address environmental safety awareness, or completing simulated work tasks such as sorting, stocking, and typing for vocation/job-related skills. Moreover, when addressing ADL and IADL skills, the occupational therapist is also incorporating skills such as problem solving, organization, planning and ideation, initiation, flexibility and regulation. These skills are important and are used regularly throughout our daily activities. Regulation is also an essential skill during the adolescent years with the various changes these individuals experience. Self regulation can help work through emotional regulation, self consciousness and negative self-talk that is often difficult during these years. Ultimately, it is the occupational therapist’s goal for each child to be as successful and independent as possible in order to participate in their daily activities and fulfill their dreams and aspirations!
Multisensory Approach to Handwriting
Handwriting is a valuable skill that doesn’t have to be taught and practiced strictly with pencil and paper! A multisensory approach to handwriting can help take away fear, pressure and the rigidness of typical handwriting practice. But what does multisensory mean? A multisensory approach to handwriting provides children with the opportunity to use their various senses (touch, visual, auditory, smell, and muscle movement) to engage in handwriting activities. How much more fun learning can be when we can incorporate a variety of textures, sounds, sights and movements to writing activities! Check out some examples of multisensory activities for handwriting below! Finger Writing in Shaving cream Painting Building letters with popsicle sticks, playdoh, clay, pipe cleaners, stickers Finger Writing in Salt, Sand, Rice or Glitter trays Finger painting Finger writing on Dry Erase markers on a window Writing with Smelly Markers Acting out the letters/big arm movements Singing letter formation during writing Writing letters in the air Chalk Writing on Bright paper, textured paper Writing to music Trace letters with a favorite toy (ex: cars, animals, small blocks, dot paint) A multisensory approach to handwriting can be helpful for all children as they all have different learning styles. Reach out to your therapist today to explore more sensory-rich experiences for your child as they practice their handwriting skills! Woodward, S., & Swinth, Y. (2002). Multisensory approach to handwriting remediation: Perceptions of school-based occupational therapists. American Journal of Occupational Therapy, 56, 305–312.
Orthotics

Karina Moore, PTA Orthotics are used for several different reasons and can be made several different ways. Pediatric orthotics can range from shoe inserts to knee high braces and more. According to Orthotics.pdf (pediatricapta.org) an orthosis is an external device with controlling forces to improve body alignment, improve function, immobilize the injured area, prevent or improve a deformity, protect a joint or limb, limit or reduce pain, and/or provide proprioceptive feedback. Orthoses are named for the part of the body they cover. Orthoses can be custom molded and custom fitted (custom fitted from prefabricated orthoses or off the shelf). There are many reasons why a child may benefit from orthotic intervention at all different ages, with and without a medical diagnosis. The use of orthotics can vary from child to child, however, the main goal is to provide stability while promoting functional ability. Orthotics or orthoses can be used to assist with pronation (rotation of the medial bones in the midtarsal region of the foot inward and downward so that in walking the foot tends to come down on its inner margin) flat feet, toe walking, weakness, poor balance, frequent tripping, leg length discrepancies, low tone, and structural issues. Orthotics are made to improve a child’s walking pattern to as normal for them as possible to facilitate age appropriate child development. Excessive pronation in the absence of high tone is usually easily corrected. A variety of “off the shelf” inserts are available, but may require customization. This type of insert is the one most commonly required. Sure Step is another commonly used orthotic. It’s not a fast fit product and must be measured. It offers wrap around support of the foot, assistance at the hind foot for position, and some assistance with ankle modulation. Open trim lines at the forefoot.”Surestep orthotics are custom-made to provide the extra support these amazing children need to run, jump and play. In fact, our core product, the patented Surestep SMO system, revolutionized orthotic management for children with pronation or low muscle tone (hypotonia) worldwide.” – Sure Step Physical therapists are trained in the function of orthoses and will frequently fit and measure orthoses. If the child is measured by the physical therapist, the orthoses are usually centrally fabricated and returned to the therapist for custom fitting and delivery. Following delivery of the orthosis, physical therapists provide education and functional training to the child and family. The physical therapists at No Limits are trained in serial casting, fitting, and measuring for orthoses. We work closely with the orthotists at Orthotics At Home to ensure a proper fit for the child’s best outcome. We also help educate the family on how to put on and take off along with a proper wearing schedule. If you are having concerns about the way your child walks, foot placement, or overall gross motor delays reach out to your pediatrician or physical therapist. We would be happy to take a look and help in any way we can. Orthotics.pdf (pediatricapta.org) Why does my child need orthotics? – ABC Pediatric Therapy Surestep–Dynamic Stabilizing System: www.surestep.net Cascade DAFO: www.cascadedafo.com
Articulation: When should I be concerned?

If you google articulation, there is a wealth of information at your fingertips. The problem, which data can you trust? Which list of developmental norms is the correct one? There are charts and blogs and articles that are all contradictory. IT is overwhelming, at best. As speech pathologists, we also see many confusing documents. This blog is meant to help parents have a quick, concise explanation based on research based articles and data from the national board for SLPs, ASHA (American Speech-Language Hearing Association). Here are some important facts: What is an articulation disorder??? An articulation disorder is defined as a speech disorder involving difficulties articulating specific types of sound Sound developmental milestones-it is important to remember that children can master these sounds early in age and many sounds have a time range of mastery Age 2: /h, p, n, d, b, w, m/ Age 3: /t, f, y, ng, k, g/ Age 4: /ch, l, v, dz, s, z, sh/ Age 5: /zh, r, th (“the”)/ Age 6: /th (“thumb”)/ If your child is not yet making these sounds, here are a few tips: How can you help improve your child’s articulation at home? Play: engage in play where you model and use lots of different sounds while playing (Example: “ch ch ch ch” as a train passes by, animal sounds, etc) Talk to your child throughout the dat to model correct production of sounds Reduce background noise when engaging with your child so there is less distraction Look at your child while you are speaking to them so they can see your model of words/sounds Read to your child Repeat your child’s sentence if it is not clear. By repeating what your child has said you are producing a good language model and you are showing that you have listened to what the child is saying What are activities to do at home to help improve articulation? Naming items together Copying facial expressions in the mirror Playing something together and modeling words they are having difficulties with Modeling and using different sounds during interactions (“s” for a snake sound, “shhh” the baby is sleeping) Listening to and identifying sounds in words (“sh” is the sound shoe starts with) Correcting if the child says a word incorrectly and having them repeat correct production back to you Finally, If you have additional concerns or want more information, reach out to your pediatrician. They will be able to listen to your child and determine if a referral to a Speech-Language Pathologist is appropriate. Early intervention is research based and helpful to many children who are not reaching the expected developmental milestones. If you have concerns, trust your instinct and talk to your doctor. NWA has many wonderful therapists that would love to help your child reach their highest potential. Happy Articulating! Miss Bailey and Mrs. Vanessa
Telehealth: Navigating New Norms
During the last year, many of us have grown accustomed to alternative ways of receiving medical care. For our therapists and other healthcare workers, they have had to find a way to prevail through the unfamiliarity and continue providing necessary therapies and treatments. Thanks to the possibility of Telehealth, No Limits Therapies and our therapists have been able to do just that. As you could expect, many of our therapists expressed some uneasiness when they were informed that some of their treatments would be conducted through a computer. Although our therapists felt immediately grateful for the opportunity to carry out necessary treatments to clients during this time, the transition was all new to them. Our therapists, whether it be an occupational therapist, physical therapist, or speech therapist rely heavily on physical cues and interactment from their clients. Our therapists soon realized they would have to become more innovative in order to determine new ways of treatment that didn’t rely on being physically present with their clients. The biggest struggles in this journey, expressed by our therapists, has been adjusting to the use of technology and things like Zoom, Google powerpoints, and other resources. With limited activities and more obstacles with technology use and limited patient interaction, they have had to set aside time to create new games and activities for their telehealth clients. Our team expressed that what normally motivated their clients in the clinic, might not have the same outcome in virtual treatment. Our therapists told us that they had to figure out what resources their kids had at home. With some kids, it was possible for them to create their own obstacle courses at home using household things like couch cushions and rolled up blankets. One of our physical therapists, Karina Moore, told us that one of her clients uses bags of dog food to walk across or jump over for an altered activity. Our therapists have learned to utilize whatever the kid has at hand. Our occupational therapist, Emily Barber, told us that her clients often use items like cans of beans, grocery bags, laundry baskets, and other common items in their telehealth sessions. Emily also told us about the positive effect of being able to track their clients eyes on the screen during Telehealth sessions for visual motor skills and processing. She explained that this is something she might not otherwise notice in a clinic session. Therapists expressed that they have not been alone in this journey as client’s parents and families have been very involved and eager to help in Telehealth sessions. With a patient that is younger, parents have been able to help their kid and the therapist by creating an obstacle course, finding access to items that could be used as alternative equipment, or encouraging their kid through treatment. Our therapists feel that they would not be able to make it through this time without such positive influence from parents and families. In turn, parents and families have been able to gain a positive impact from the experience as well. By being more involved, they have been able to encourage their kids more frequently and effectively. By having the opportunity to witness their child’s session from home, they have been able to pick up on activities that they could do with their kid outside of treatment sessions. Our therapists have been able to work with the parents and families directly and discuss their kids development first hand. This benefit has been impeccable to the overall support of a patient as well as their progression and well being.
Reflexes?!?! What is the big deal?
If you have been around No Limits Pediatric Therapies long, you have probably heard one of the occupational therapists mention “primitive reflexes.” You may be wondering what is a primitive reflex? And what is the big deal? According to Webster Dictionary, a reflex can be defined as “an automatic and often inborn response to a stimulus that typical involves a nerve impulse passing inward from a receptor to the spinal cord and then passing outward from the spinal cord to an effector (such as a muscle or gland) without reaching the level of consciousness and often without passing to the brain.” For this blog post, we will be focusing on primitive motor reflexes and how they can impact your child’s function. According to the Medical Dictionary, a primitive reflex is defined as “any of various simple, stereotypic, automatic neuromuscular responses characteristics of the mature fetus and newborn but typical inhibited (or integrated) during the first year of life: primitive reflexes are directed by the brainstem centers and include Moro, rooting, and tonic neck reflexes.” It is thought that these reflexes help infants learn to organize motor behavior. Integration can be defined as “the inhibition by higher centers of neurological control which modify the reflex in such a way that the pattern of response is no longer stereotypical. The reflex does not disappear; it may reactivate under stress or during activities requiring great strength.” If these so called “primitive reflexes” continually remain to be displayed beyond the expected of typical developmental time period, their presence by indicate an underlying developmental of neurological issue. When a child’s primitive reflexes do not integrate, they may interfere with a child’s development of more advanced motor skills, which could lead to difficulty participating in one home, educational or community environments to their highest potential. Now, let’s take a look at the three primary tonic reflexes: Asymmetrical Tonic Neck Reflex (ATNR): Onset: 0-2 months Integration: 4-6months Stimulus: Rotation of the head Response: Arm and leg on the “jaw” side extends. Arm and leg on the “skull” side flex. Importance for Baby: Assists with early eye-hand regard, provides vestibular stimulation, changes the distribution of muscle tone. Significance on Early Development if Persists: May impair ability to roll, use hands smoothly together at midline, poor visual regard for object(s) being held, poor balance. May impair creeping or crawling. Baby loses balance and/or falls when rotates his head from midline; very frustrating and causes excessive fatigue. Symmetrical Tonic Neck Reflex (STNR): Onset: 4-6 months Integration: 8-12 months Stimulus: Flexion and extension of the head (neck) Response: With neck flexion the upper extremities will flex and the lower extremities will extend. With neck extension the upper extremities will extend and the lower extremities will flex. Importance for Baby: The STNR assists in the development of bilateral patterns of body movement. Allows the child to move up against gravity and assume quadruped (on all fours like a dog). Integrates as the child begins to crawl and can lift the buttocks from the heels without flexing the neck. Integrated when rocking back and forth on hands and knees. Significance on Early Development if Persists: Interferes with advanced reciprocal creeping. Impairs dissociation between the two lower extremities and transitioning between quadruped to sitting to kneeling to standing and vice versa. If strongly influenced by the STNR a baby will not be able to creep; will bunny hop versus true creeping/crawling on the floor. Tonic Labyrinthine-Prone & Supine (TLR): Onset: Birth Integration: 6 months Stimulus: Change of orientation of the head in space; position of head in relation to gravity while prone (on belly) and supine (on back). Response: In prone flexor tone will predominate with arms flexed by the child’s chest. In supine extensor tone will predominate. Importance for Baby: Allows the baby’s posture to adapt to that of the head. Significance on Early Development if Persists: Will interfere with movement that requires smooth grading of flexor and extensor muscles. In supine child will have a compromised ability to raise their head up against gravity; this will affect anti-gravity control for movements such as bringing feet and hands together and rolling. In prone (on belly) child will have compromised ability to raise head, extend spine, and bear weight on elbows. This, in turn, will limit time spent on his/her tummy for crawling and developing the movement in their pelvis and shoulders that sets the stage for moving in and out of various body positions (sitting to stand). Without such ability, the baby will be without options for exploring. This will affect social and cognitive gains. (Above graphics from “Primitive Motor Reflexes & Their Impact on a Child’s Function”) Now that we have reviewed tonic reflexes, how can the presence of these primitive reflexes effect your older child? Influences of Retained Asymmetrical Tonic Neck Reflex (ATNR): Poor isolation of individual body movements Pore sitting posture Attention & Focus Impaired pre-writing and writing Impaired scissor use Fasteners/Typing/Musical Instruments Impairments in reading Keyboard Use Impairment in gait (walking) Running Influences of Retained Symmetrical Tonic Neck Reflex (STNR): Decreased strength and balance Sitting Floor Sitting Walking Writing Ball handling skills Influences of Retained Tonic Labyrinthine Reflex (TLR): Walking Sitting Writing Balance Now, we have discussed primitive reflexes and how they may present in your older child; as well as the difficulties they may lead to. Let’s look at some activities to help integrate these reflexes. Prone for fine motor activities & games- The elbows provide a point of stability for freeing the hands for manipulating. Hold a large dowel with both hands, use this to push a ball back and forth Use arms to push a ball back and forth Color, paint, draw, read, or complete puzzle in prone Use whistles or play games that require blowing through a straw Pivot in both directions Prone on therapy ball, platform swing, or over bolster Prone on scooter board-push off with arms from wall to glide backward Prone on scooter board-being pulled by a rope while grasping onto it with both hands Superman/SuperWoman – prone extension with arms
Benefits of Heavy Work Activities

Benefits of Heavy Work Activities Emily Barber, MS, OTR/L With the craziness and busyness of summer and schedule changes, our bodies can often become disorganized, we can become more anxious and stressed due to ever-changing schedules, and lose focus and attention easier. A child experiencing this may accidentally breaks things often, appear clumsy and uncoordinated, and may have a lot of energy with the excessive need to crash and bump into objects, walls and/or people. Children seeking these movements may be seeking input to calm and organize their bodies. Heavy work activities, which are simply any type of action that pushes or pulls against the body, can help provide the deep pressure input they are craving and allow them to move their bodies in a safe way. Heavy work activities provide proprioceptive input to the joints and muscles. Proprioception is about knowing where your body is in space. Problems within our proprioceptive system occur when the messages that tell a child where he is, how to move, and how much effort to exert aren’t as strong. Proprioceptive input, or deep pressure input, can be very calming, organizing, and regulating to the body and can decrease stress and anxiety through heavy work activities. Heavy work can also increase body awareness, focus and attention. Heavy work activities might include: • Animal walks • Jumping on the trampoline • Swimming • Playing with play dough (kneading, pulling, squeezing) • Climbing on the jungle gym • Doing the monkey bars • Blowing bubbles • Jumping jacks • Push-Ups • Riding a Bike • Creating an obstacle course • Doing Yoga • Pulling a heavy wagon • A pillow fight • Running through the sprinkler • Tug of War • Carrying beanbags or weights around the house • Rock climbing • Hop-Scotch When your child appears to be craving proprioceptive input and “bouncing off the walls,” provide them with some heavy work activities! Ask your occupational therapists at No Limits Pediatric Therapies for additional suggestions or about heavy work benefits for your child!
